what are the human clinical issues linked to the increasing use of antibiotics in animal feed
Effects of Antibiotics on Animal Feed
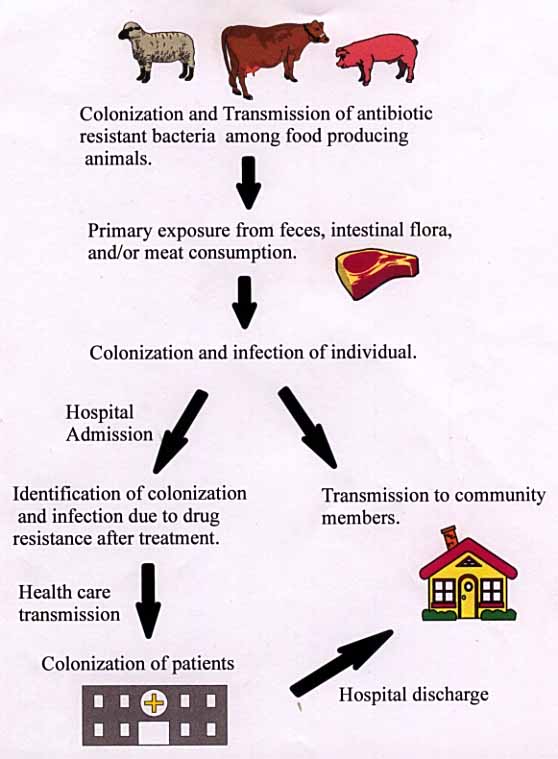
Flowchart
Use of Antibiotics in Animal Feed
Antibiotics take been used in animal feed for about 50 years e'er since the discovery not only every bit an anti-microbial agent, simply likewise every bit a growth-promoting agent and comeback in operation. Tetracyclines, penicillin, streptomycin and bactrican soon began to exist common additives in feed for livestock and poultry. Currently, the following antibiotics are used in livestock and poultry feed: chlortetracycline, procaine penicillin, oxytetracycline, tylosin, bacitracin, neomycin sulfate, streptomycin, erythromycin, linomycin, oleandomycin, virginamycin, and bambermycins. In addition to these antibiotics, which are of microbial origin, at that place are other chemically synthesized antimicrobial agents that are besides sometimes used in animal feeds. These include 3 major classes of compounds: arsenical, nito-furan, and sulfa compounds. Arsenical compounds include arsanilic acid, 3-nitro-4-hydroxy phenylarsonic acid, and sodium arsanilate; nitro-furan compounds include furazolidone and nitro-furazone; sulfamethazine, sulfathiazole, and sulfaquinoxaline. Other chemicals are also used as antiprotozoal agents to forestall coccidiosis and histomaniasis in chickens and turkeys. Antibiotics are used regularly in animate being feed at a rate of 2 to l grams per ton for improved functioning in the animals. The reasons include a more than efficient conversion of feed to animal products, an increased growth rate and a lower morbidity/bloodshed rate in general. The levels of antibiotics are oft increased to fifty-200 grams/ton or more when specific diseases are being targeted as when the spread of a particular disease is rampant. The levels are besides increased in times of stress. This increased amount is often decreased when the threat of a affliction is gone. Benefits of Antibody use in Animal Feed
The benefits of antibiotics in animal feed include increasing efficiency and growth rate, treating clinically sick animals and preventing or reducing the incidence of infectious disease. By far the major use of antibiotics among these, however, is increased efficiency, i.e. a more efficient conversion of feed to animal products, and an improved growth rate. In chicken feed, for example, tetracycline and penicillin evidence substantial improvement in egg production, feed efficiency and hatchability, just no significant effect on mortality. Chlorotetracycline, oxytetracyclin and penicillin also show an improved growth charge per unit, but little upshot on mortality. Antibiotics in animal feed, in general, are used regularly for increased efficiency and growth rate than to gainsay specific diseases. Risks of Antibiotics in Animal Feed
After animals have been fed antibiotics over a period of fourth dimension, they retain the strains of bacteria which are resistant to antibiotics. These bacteria proliferate in the fauna. Through interaction, the resistant leaner are transmitted to the other animals, thus forming a colonization of antibiotic resistant bacteria. The bacteria flourish in the intestinal flora of the animal, also equally, in the muscle. Every bit a result, the carrion of the animal often comprise the resistant bacteria. Transfer of the bacteria from animal to human is possible through many practices. The primary exposure of humans to resistant bacteria occurs in farms and slaughterhouses. Humans clean the feces, which contain the leaner, of the animals on farms. During the cleaning process, humans may get bacteria on their torso and hands. If the body or hands are not properly cleaned, the bacteria could be ingested by the person. Likewise, in slaughterhouses, during slaughter, the intestine is severed. Resistant leaner are exposed to slaughterhouse workers, which could get the bacteria on their bodies and hands. Manual occurs when the leaner is ingested. Along with the previous sources of contamination, humans can get infected past eating meat from animals with resistant bacteria. Even though cooking reduces the survival of the bacteria, some may still survive and infect the human. For instance, 1983, 18 people in 4 midwestern states developed multi-drug resistant Salmonella food poisoning subsequently eating beef from cows fed antibiotics (one). After initial transmission and infection to humans, the transmission to other humans has a couple paths. Transmission can take place through the many mediums (droplets, physical contact, and bodily fluids) of human contact in the customs. An infected private may also be admitted to a hospital for treatment. Treatment may non work in drug resistant leaner, therefore, identifying a drug resistant infection. Bacteria is transmitted to other patients via the hospital environment or wellness care worker=due south hands. Later on manual, the leaner will colonize in several of the patients. Colonization in other patients with other resistant leaner can produce bacteria with multi-drug resistance. One time the patients recover, they are discharged into the community. These patients could potentially infect several customs members. Multiple infection could potentially produce a supergerm which is resistant to many drugs due to resistance sharing between bacteria. General Resistance Inforamtion
In about cases, the drug resistance genes of leaner are carried on plasmids (specifically, the R or resistance plasmid), which replicate separately from the cell�s circular DNA. These plasmids tin can exist passed from prison cell to cell, allowing for a drug resistance to be passed to a big group of leaner and to different types of leaner. These resistance genes are besides carried on transposons, which permit for these genes to move from one strand of genetic textile to another. Because of this, a cell can receive multiple plasmids with resistance genes and and so integrate all of the resistances onto one plasmid. Some R plasmids have every bit many as eight drug resistances on them. Rise of Resistance
The development of a drug resistance is not orchestrated specifically to counteract a drug. Rather, drug resistances arise because of spontaneous genetic mutations within a gene sequence. By chance, these mutations happen to produce some change in the cell that allows for drug resistance. This mutated bacteria and then has a selective advantage over other not-resistant bacteria. The add-on of antibiotics to the environment (the host organism) then selects for the resistant bacteria by killing off all of the not-resistant leaner. This allows for the resistant cells to abound and divide, creating a large population of resistant bacteria. The larger population then increases the likelihood that plasmid transfer will occur to other, non-resistant bacteria of various strains. This attained resistance has little effects on the host organism until plasmid/resistance transfer to a particularly virulent bacteria occurs. And then, the host is susceptible to infection from this organism without the benefit of treatment with the antibody that the bacteria is at present resistant to. Mechanisms of Resistance
There are several general methods through which a prison cell can get resistance to an antibiotic. These mechanisms are: - 1. Decreased cell permeability to the drug - the prison cell tin change its membrane structure so that the drug cannot enter the prison cell and perform its function
- 2. Modify the drug binding/recognition site - past changing the construction of the membrane surface, the site which previously allowed the drug to bind to the cell can no longer do and so
- 3. Chemic modification of the antibiotic - by cleaving a portion of the molecule or calculation a substituent group, the backdrop of the agile molecule in the antibiotic can be altered such that it is rendered harmless to the cell
- 4. Active transport - the ship of drug molecules out of the cell. In many cases, this is washed via a drug/proton antiport system. With this mechanism, H+ ions are pumped into the cell as drug molecules are pumped out.
- 5. Enzyme or pathway alteration - the cell can modify the pathway or enzyme used to carry out a prison cell process occurs. By doing this, the cell can featherbed the enzyme that is affected and cause the drugs effects to have no bearing on the functioning of the prison cell.
Methods of Plasmid Transfer
In that location are iii principal ways in which genetic material (in this case, drug resistance genes) tin can be exchanged betwixt leaner. They are as follows: - 1. Conjugation - a direct, cell-to-prison cell, contact transmission method. The plasmid containing prison cell generate a minor tubule that connects the 2 cells (the sex pili). This tube then allows for the passage of DNA strands between the 2 cells
- 2. Transformation - the absorption of "naked", free-floating Dna by a cell. Upon the death of a bacterial jail cell the cell components degrade, leaving the Deoxyribonucleic acid and cell materials to disperse in the environment. If a cell with antibiotic resistance dies and breaks down, the resistance gene may be released into the environment and absorbed past another bacterial cell.
- 3. Transduction - the transportation of genetic material by a bacteriophage. When a bacteriophage infects and replicates in a prison cell, some new phages may be filled with cellular genetic cloth, rather than viral genetic material. In some cases, this cellular material is a resistance factor. When the phage containing the resistance cistron infects another cell, the infected cell then gains the bacterial resistance.
Economical Bear on
The economic impact is difficult to measure, partly because all-encompassing searching could non turn up verbal figures for employees and profits specifically in feed additives. However, it is prophylactic to say that in the U.Due south. alone, stopping the practice of calculation antibiotics would consequence in a loss of millions of dollars in profits and thousands of lost jobs. It is also worth noting that sales of antibiotics are a very profitable sector for companies that engage in their productions. References
- Antibiotics in Brute Feed, Council for Agricultural Science and Technology, 1981.
- McDonald, L. Clifford, Matthew J. Kuehnert, Fred C. Tenover, and William R. Jarvis (1997). "Vancomycin-Resistant Enterococci Exterior the Wellness-Care Setting: Prevalence, Sources, and Public Wellness Implications" Centers of Disease Control and Prevention, Alanta, Georgia, 3.
wysiwyg://67/http://www.cdc.gov/ncidod/EID/vol3no3/mcdonald.htm - "The Rise of Antibody-Resistant Infections" (1995). FDA Consumer, 29.
http://www.fda.gov/fdac/features/795_antibiotic.html
Return to Introduction Page.
Source: https://www1.udel.edu/chem/C465/senior/fall97/feed/present.html
0 Response to "what are the human clinical issues linked to the increasing use of antibiotics in animal feed"
Post a Comment